Osteoporosis is a common and serious condition which occurs in both men and women, although unequally. 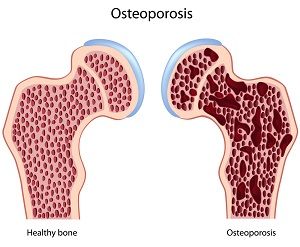 According to the American Academy of Orthopedic Surgeons, approximately 10 million people in the U.S. have osteoporosis and 80 % of them are female.
According to the American Academy of Orthopedic Surgeons, approximately 10 million people in the U.S. have osteoporosis and 80 % of them are female.
Literally meaning “porous bone”, the honeycomb-like holes in the trabecular part of the bone become enlarged due to bone loss. This loss of bone mass weakens the bone which can then easily fracture from even a minor fall. This also happens when too little bone is being made to replace what is lost.
While bone loss can slowly happen over time from about age 30 on, during midlife the rate of bone loss generally increases. With menopause, the level of estrogen in women drops sharply, and this allows the osteoclast to become more active breaking down bone. So much so that women can lose 20% or more of their bone density in the 5 – 7 years following menopause.
Osteoporosis can be categorized as either primary or secondary. Women generally have primary osteoporosis, meaning it is mostly due to age, or menopause. Secondary osteoporosis is generally diagnosed in men, and is a result of medications, endocrine or inflammatory disorders, or disease of the bone marrow.
Risk Factors
The National Osteoporosis Foundation lists the following risk factors for osteoporosis:
– female
– advanced age
– family history of having osteoporosis or breaking bones
– small thin frame
– being of Caucasian, Asian, or Latino descent
– post menopause
– low estrogen and/or testosterone levels
– bedridden or sedentary lifestyle
– smoking
– drinking excessive amounts of alcohol
– taking medications that can harm bones
– having other health conditions that can harm bones
The American Academy of Orthopedic Surgeons adds:
– insufficient calcium in the diet
– Vitamin D deficiency
Screening & Diagnosis
The U.S. Preventive Services Task Force recommends “…screening for osteoporosis in women aged 65 years and older and in younger women whose fracture risk is equal to or greater than that of a 65-year old white women who has no additional risk factors”. Healthcare providers may recommend screening for other reasons such as for clients who are over 50 and have broken a bone from a minor injury, or have more than one risk factor.
Osteoporosis can only be diagnosed with a bone mineral density (BMD) test. This test will measure the amount of bone density in certain areas of bone, generally the hip and spine. The recommended test uses a DXA (dual energy x-ray absorptiometry) machine, which is a very low dose x-ray and takes about 15 minutes. The machine will give a T-score that describes the difference between the bones tested and the bones of a young healthy adult. Per the National Osteoporosis Foundation, a score of +1 to -1 indicate healthy bones. A score of -1 to -2.5 indicates bone density that is lower than normal, termed osteopenia, but not osteoporosis. A score of -2.5 or lower indicates a diagnosis of osteoporosis.
Many people with osteoporosis are not diagnosed until they have fractured a bone. There are no other signs or symptoms that would indicate this disease. Speak to your health care provider to see if a BMD test is appropriate for you.
References: American Academy of Orthopaedic Surgeons; National Osteoporosis Foundation; US Preventive Services Task Force